FDA ‘commencing a study’ that could lead to the removal of a once-lifetime ban on gay men donating blood as COVID-19 survivor says he was turned away from blood center for being gay
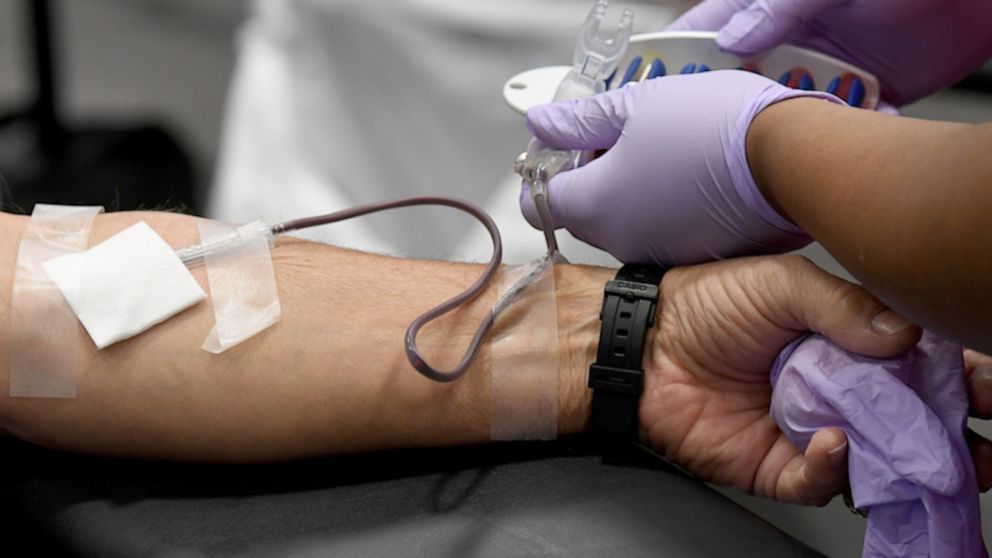
“You won’t be donating today.”
Reverberating words to hear for a man who just recovered from COVID-19, who claims he was turned away from donating his plasma on the basis of his sexual orientation.
In a now-viral Facebook post, 36-year-old Lukus Estok says he was selected by a New York City hospital as a prime candidate with a high antibody count to take part in potentially life-saving coronavirus research around blood plasma and COVID-19 antibodies.
“I was subsequently put through two separate (but identical) rounds of donor screening questions,” Estok wrote. “I answered the questions honestly. The New York Blood Center scheduled an appointment for me to donate my plasma.”
1:57GLAAD president and CEO, Sarah Kate Ellis, says revised FDA blood donation deferral policy is still steeped in stigma for gay and bi-sexual men.
Estok, who lives in New York City, told “GMA” in an interview, “I was excited, nervous, very nervous, because I haven’t really had any experience donating blood since I was 18.”
“After going through that illness and everything that it put me through, the last thing I wanted to do was leave someone else out there who didn’t need to be suffering as badly as they were right now without an option,” Estok said.
“I went from feeling like I had to like dry cough to feeling like someone was sitting on my chest. I had trouble breathing to the point where when I walked to the bathroom, I got dizzy and that’s when I got very nervous and very panicky because I have asthma,” he said.
Estok described that while he was in the waiting room with other potential donors, staff inquired why he hadn’t donated blood since he was 18. Estok says the atmosphere changed completely when he volunteered the information that he is a gay man.
“At that moment, the facial expression, even with a mask on in the look of the eyes of the person I was talking to, completely changed. And without any hesitation, the response back to me was, ‘well, you will not be donating today,’” Estok said.
“I was disappointed in myself for volunteering that information,” he told “GMA.”
Estok added that while he attempted to defend his candidacy as a donor, the blood center staff retorted, “I don’t know what you think you know, but you will not be donating, here, today.”
“All I wanted to do was help,» he echoed.
“In that moment, not only was I not allowed to help, but I was in front of other people being told that I wasn’t worthy of the donation, that I wasn’t fit to be there.”
A ban on gay blood
Facts show that Estok’s experience, despite being surfaced as a prime candidate for antibody research and plasma recovery after being infected with COVID-19, is consistent with federal guidelines set by the Food and Drug Administration (FDA), “to reduce the transmission of HIV by blood and blood products.”
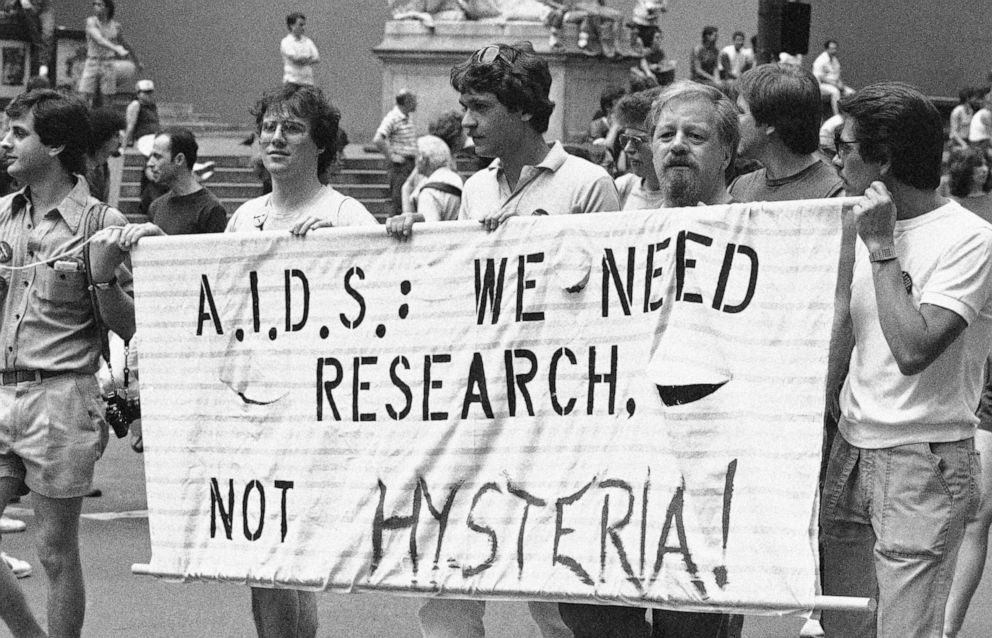
A restriction born out of the HIV/AIDS crisis of the 1980s when limited testing technology existed to screen blood for HIV, the FDA initially implemented a lifetime ban, in 1983, on blood donations from all men who had sex with men after 1977.
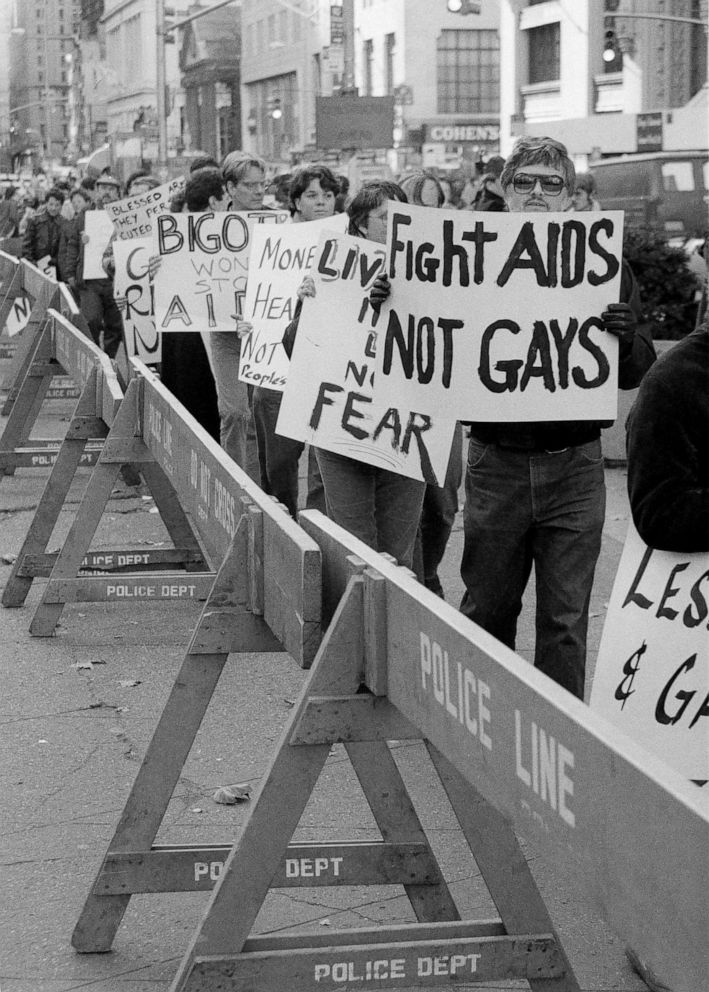
That policy was upheld until 2015, when the FDA revised the guidelines from a lifetime ban to a 12-month deferral period. Meaning, gay and bisexual men had to abstain from having sex with another man for at least 12-months before being allowed to give blood.
On April 2, amid the COVID-19 crisis and calls from the Surgeon General for healthy Americans to give blood and avert a national shortage, the FDA revised the 12-month deferral period down to 3-months.
These most-recently revised guidelines for gay and bisexual men also extend to women who have had sex with men who have sex with other men, as well as anyone who has had recent tattoos and piercings.
Effectively, the revised FDA 3-month deferral period guidelines include gay and bisexual men who are in a monogamous relationship, gay and bisexual men who are practicing safe sex as well as gay and bisexual men who are HIV-negative.
By comparison, a straight man who is in a polygamous relationship or engages with multiple female sex partners has no outright restrictions on giving blood based on his sexual activity.
While the FDA statement says the data by which the decision was made to revise the deferral period brought on by a global pandemic was, “based on recently completed studies and epidemiologic data,” many doctors across the U.S. claim that any deferral period in 2020 is not only stigmatizing for the LGBTQ+ community overall, but is limiting the nation’s ability to relieve itself from a critical blood shortage.
Risk vs. stigma
“Really, what it comes down to is it seems like just that stigma is lingering and that’s why this policy is still there,” Dr. Monica Hahn of U.C. San Francisco Health told “GMA.”
Dr. Hahn, a Family Physician, specializes in HIV Prevention and Management and reiterated how far science has come in the last decades.
“These bans were made because it was a frightening time where we just didn’t have the testing technology to adequately screen our blood supply,” Hahn told “GMA.”
“It would take several months after someone acquired HIV for it to show up on a test because your body needs time to make antibodies in reaction to the HIV virus. But, if you fast forward to today with our newer tests, the window period is really reduced to just about 10 days, meaning that we can really accurately detect the presence of HIV in patients about 10 days after HIV transmission occurs. The onus is on our screening system and I really believe that people are being discriminated against.”
“There’s really no scientific reason anymore, in my opinion, to have this ban at all since our testing capacity has been truly revolutionized,” Dr. Hahn added.
Dr. Hahn told «GMA» that the U.S. is already behind, pointing out that countries like Italy and South Africa have already moved to what’s called an “individual risk assessment,” in regards to reducing the transmission of HIV by blood and blood products.
According to the U.S. National Library of Medicine National Institutes of Health, «Italy moved from a permanent deferral for ‘men who have sex with men’ to an individual risk assessment of sexual behaviors,” in 2001.
“What that risk assessment policy does — it just makes a lot more sense. And it’s that they ask the same questions about risk behaviors of everybody, regardless of sexual orientation,” Dr. Hahn told “GMA.”
Dr. Patrice Harris, President of the American Medical Association (AMA) agrees with Dr. Hahn and told «GMA,» “risk-based approach would also be data-driven.”
“A questionnaire would ask about recent sexual history, whether the potential donor has recently injected non-prescription drugs, perhaps even recently had or been in contact with someone who has an infectious disease,” Dr. Harris said.
“The AMA has been a long-term advocate of using a risk-based approach rather than stigmatizing one group of people. So we believe there should not even be the three-month deferral, but that we should use a risk-based approach,” Harris told “GMA.”
Despite the series of loosening FDA guidelines over the years, the fact remains they are unequivocally that, guidelines rather than mandates.
The onus of implementation falls directly on the blood centers, which are not required by federal law to implement revised guidelines at all. Further, the FDA informed «GMA» that a blood center could choose to have stricter policies than the FDA, but not looser ones. Meaning, blood centers are within their right to uphold FDA guidelines of years and decades past.
Calls for action
Dr. Hahn has found she is not the only one that feels the FDA is overdue to remove the deferral policies surrounding gay and bisexual men. In an open letter she co-authored with UCSF colleague Dr. Deborah Cohan, they press the FDA “for scientifically-driven standards that uphold the utmost safety of the blood supply and simultaneously promote equity and reverse historical discrimination in blood donation.”
Over 500 medical professionals have co-signed their open letter.
Stars such as Sam Smith and Margaret Cho joined over 24,000 who have shown their support for a petition, launched by LGBTQ+ advocacy group GLAAD, to also press the FDA to remove the outdated guidelines as they claim.
“The FDA’s decision to lower the deferral period on men who have sex with men from 12 months to 3 months is a step towards being more in line with science, but remains imperfect,” GLAAD president Sarah Kate Ellis told “GMA.”MORE: «GLAAD Pres. and CEO speaks out on revised FDA blood deferral policy»
In an op-ed, Human Rights Campaign president Alphonso Davies reiterated the position that the blood deferral policy of today is “still rooted in stigma and bias.” Adding that, “a truly bias-free deferral policy should be based on information that is within the personal knowledge and control of the prospective donor—and not on the sexual orientation or gender identity of the donor, or the sexual orientation, gender identity, or activities of one’s sexual partners, or on perceived monogamy.
TV host Andy Cohen got personal on his show “Watch What Happens Live” to share that he too was turned away for plasma recovery after signing up for a program for COVID-19 survivors to help those battling the virus now.
“Why are members from my community being excluded from helping when so many people are sick and dying?” Cohen asked.

On being turned away
In the case of Lukus Estok’s experience, even though he was referred to by a hospital system that deemed him a top candidate for COVID-19 antibody research and plasma recovery, New York Blood Center was rendered incapable of accepting his blood because they had yet to implement the updated FDA guidelines.
America’s Blood Centers, the organization that operates North America’s largest network of community-based, independent blood programs like New York Blood Center also told “GMA” to throw caution at the term “immediate effect” used by the FDA when describing how policy revisions are implemented. They add that it’s doubly confusing for the public.
“The word ‘immediate’ means that blood centers may begin the process of implementing the changes, all of which happens in a regulated and controlled environment. For a blood center, this means significant updates to an FDA-reviewed donor history questionnaire, SOPs/procedures, computer systems, and trainings. Blood centers also will need to validate their procedures, computer systems, and trainings,” America’s Blood Centers CEO Kate Fry told “GMA.”
A spokesperson for New York Blood Center, where Estok was expecting to give convalescent plasma, explained to “GMA” that the process of implementation of revised FDA guidelines is not a swift action. “We’re working as quickly as possible and hope to finish implementing them by mid-May,” the spokesperson said.
According to Estok, “It’s not like flipping a light switch,’ they explained to me.»
“Exciting news for me; in just a few short months, I’ll still be me,” he said.
Asked whether Estok would have been able to give blood or plasma based on an individual risk assessment, New York Blood Center did not comment.
The New York Blood Center spokesperson told “GMA,” “we’ve been in contact with the donor [Lukus] to discuss how we can further improve our donor engagement processes. We would love to work with him to advocate for further change, and we would welcome him to come back and be at the front of the line when we begin accepting newly eligible donors in the coming weeks.»
What happens now?
In a statement, an FDA spokesperson told “GMA,” “the FDA is committed to considering alternatives to the time-based deferral for men who have sex with men by generating the scientific evidence that will support an effective individual risk assessment-based blood donor questionnaire.”
The FDA goes on to reveal to “GMA” they are, “working to commence a pilot study that will enroll about 2000 men who have sex with men and who would be willing to donate blood.”
“This study, being conducted at community health centers in key locations across the United States, could generate data that will help the FDA determine if a donor questionnaire based on individual risk assessment would be as effective as time-based deferrals in reducing the risk of HIV.”

This is the first time the FDA has made public mention of a study to work toward moving to an individual risk-based assessment for blood donors and the would inevitably remove the once-lifetime ban on gay and bisexual men from giving blood or blood products and any deferral period thereafter.
Until that time comes, the FDA blood deferral policy for gay and bisexual men stands on its current 3-month deferral period.
“Three months is still an unacceptable barrier to ask a certain section of the population and not the rest of the population to have to clear,” Lukus Estok told “GMA.”
“We don’t need old stigma dictating the way that we make medical and scientific decisions. That’s not how it’s supposed to work. Science is supposed to inform the way we make decisions.”





